ATI IV therapy and peripheral access are essential techniques in healthcare, enabling the administration of medications, fluids, and other therapies directly into the bloodstream. This article provides a comprehensive overview of these procedures, discussing their principles, indications, complications, and best practices.
ATI IV therapy involves the insertion of a small catheter into a vein, allowing for the delivery of medications and fluids directly into the bloodstream. Peripheral access, on the other hand, refers to the establishment of a temporary connection to a peripheral vein, typically in the arm or hand, for the purpose of administering medications, drawing blood, or providing fluids.
ATI IV Therapy
ATI IV therapy involves administering medications or fluids directly into a vein through a peripherally inserted central catheter (PICC). This technique provides long-term vascular access, typically for several weeks to months, and is commonly used in patients requiring extended IV therapy.
The principles of ATI IV therapy include:
- Insertion of a PICC line through a peripheral vein, typically in the upper arm.
- Advancement of the catheter into a central vein, usually the superior vena cava.
- Securement of the catheter to prevent dislodgement.
Indications for ATI IV therapy include:
- Long-term administration of medications or fluids.
- Patients with difficult peripheral venous access.
- Patients requiring multiple IV medications or blood transfusions.
Contraindications to ATI IV therapy include:
- Infection at the insertion site.
- Thrombosis of the central veins.
- Severe coagulopathy.
Case studies have demonstrated the successful use of ATI IV therapy in patients with cancer, chronic infections, and other conditions requiring prolonged IV treatment.
Peripheral Access
Peripheral access refers to the establishment of a connection to a peripheral vein, usually in the arm or hand, for the administration of medications, fluids, or blood transfusions.
Methods and techniques for establishing peripheral access include:
- Venipuncture: Using a needle and syringe to puncture a vein.
- Peripheral IV catheterization: Inserting a small plastic tube (IV catheter) into a vein.
- Midline catheter: Inserting a longer catheter into a vein in the arm, typically for medium-term access.
A comparison table of peripheral access devices is provided below:
| Device | Advantages | Disadvantages |
|---|---|---|
| Venipuncture | Simple and quick to perform | Limited duration of access |
| Peripheral IV catheter | Versatile and can be used for short-term to medium-term access | Higher risk of infiltration or extravasation |
| Midline catheter | Provides medium-term access and is less likely to cause infiltration | More difficult to insert and maintain |
Proper peripheral access maintenance involves:
- Regular assessment of the IV site for signs of infection or infiltration.
- Securement of the IV catheter to prevent dislodgement.
- Dressing changes to keep the site clean and protected.
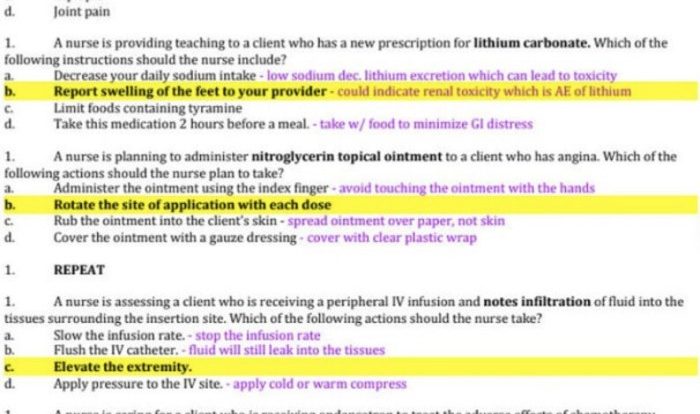
Troubleshooting peripheral access problems may include:
- Infiltration: Leakage of fluid into surrounding tissues.
- Extravasation: Leakage of medication or fluid outside the vein.
- Phlebitis: Inflammation of the vein.
Complications of ATI IV Therapy and Peripheral Access
Potential complications associated with ATI IV therapy and peripheral access include:
- Infection at the insertion site.
- Thrombosis of the vein.
- Infiltration or extravasation of fluids or medications.
- Phlebitis.
- Catheter dislodgement.
Strategies for preventing and managing these complications include:
- Strict adherence to aseptic technique during insertion and maintenance.
- Regular assessment of the IV site for signs of infection or infiltration.
- Prompt treatment of any complications that arise.
Patients should seek medical attention if they experience any of the following:
- Redness, swelling, or pain at the IV site.
- Leakage of fluid or medication from the IV site.
- Chills or fever.
Best Practices for ATI IV Therapy and Peripheral Access

Best practices for administering ATI IV therapy and establishing peripheral access include:
- Assessment of the patient’s condition and selection of the appropriate access method.
- Proper insertion and securement of the IV catheter.
- Regular monitoring of the IV site for signs of infection or infiltration.
- Documentation of all procedures and observations.
- Communication with the healthcare team and patient about the IV therapy and peripheral access.
Nursing assessment and monitoring play a crucial role in ensuring patient safety during ATI IV therapy and peripheral access. Nurses are responsible for:
- Assessing the patient’s condition and selecting the appropriate access method.
- Inserting and securing the IV catheter.
- Monitoring the IV site for signs of infection or infiltration.
- Documenting all procedures and observations.
- Communicating with the healthcare team and patient about the IV therapy and peripheral access.
Guidelines for documentation and communication related to ATI IV therapy and peripheral access include:
- Documenting the date and time of insertion.
- Documenting the type of IV catheter used.
- Documenting the location of the IV site.
- Documenting any complications that arise.
- Communicating with the healthcare team and patient about the IV therapy and peripheral access.
Quick FAQs
What are the indications for ATI IV therapy?
ATI IV therapy is indicated when rapid administration of medications or fluids is necessary, when oral administration is not feasible, or when sustained delivery of medications is required.
What are the potential complications of peripheral access?
Potential complications of peripheral access include infection, hematoma, infiltration, and nerve damage. Proper technique and maintenance are essential to minimize these risks.
When should medical attention be sought for complications of ATI IV therapy or peripheral access?
Medical attention should be sought immediately if any signs of infection, such as redness, swelling, or drainage, occur at the IV site. Additionally, if the IV line becomes dislodged or the patient experiences pain, discomfort, or swelling at the peripheral access site, medical attention should be sought promptly.